In In-depth
Follow this topic
Bookmark
Record learning outcomes
Endometriosis care in the UK is in a desperate state. Women are facing wait times for diagnosis of close to a decade. Those with an intuit that they may have the condition are often being dismissed by healthcare professionals as having severe period pain. When it comes to the time for those affected to try and conceive, the impact of years of misdiagnosis, lack of treatment and the emotional toll can, too, provide fertility challenges.
More attention needs to be paid to this condition that affects one in 10 people whose sex was recorded female at birth, especially considering its symptoms include chronic fatigue, chronic pelvic pain and difficulty conceiving. The Ovum 2025 Endometriosis Report is doing just that, and the findings are startling.
The long road to diagnosis
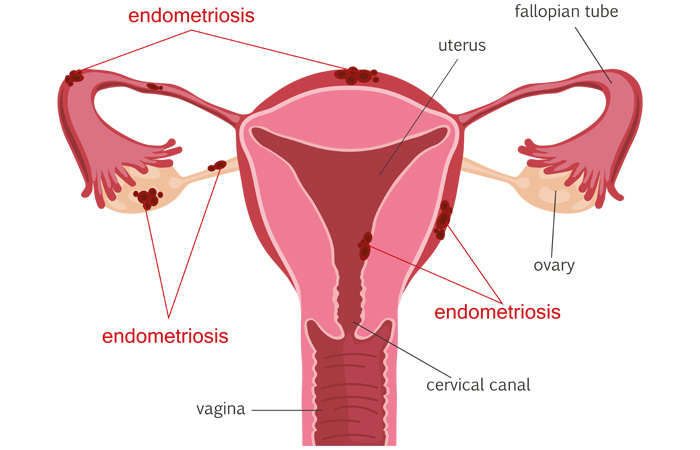
Endometriosis is a disease which affects women and those with a uterus of reproductive age. The tissue similar to the lining of the uterus grows outside the uterus, which leads to inflammation and scar tissue forming in the pelvic region, causing severe pain that can be debilitating. It is especially apparent during menstruation, sexual intercourse, urination and/or bowel movements. The cause of endometriosis is unknown, and while symptoms can be treated, there is currently no cure.
“Endometriosis care in the UK has seen increased public awareness in recent years, which is fantastic to see, and that momentum must be maintained, but unfortunately, significant challenges remain,” says Jenny Wordsworth, CEO and founder of Ovum – an organisation providing support for those affected by endometriosis. “While some progress has been made, many patients still face a long and frustrating journey to diagnosis and treatment.”
The report, which surveyed hundreds of people with endometriosis, found that 38 per cent waited over eight years for a diagnosis, while a further 19 per cent waited four to seven years. Some 72 per cent of respondents saw over three healthcare professionals before receiving a diagnosis, while an alarming 62 per cent were dismissed or told that their pain was ‘normal’ before being diagnosed.
“It currently takes on average nearly nine years to get a diagnosis of endometriosis in the UK – a statistic that hasn’t changed in over a decade,” says Faye Farthing, head of communications at Endometriosis UK.
“Lack of awareness and education among public and health practitioners are among contributory factors. Gynaecology waiting times also remain unacceptably high.” Jenny echoed Faye’s concern around the knowledge gap of healthcare professionals contributing to this long wait time.
“The biggest blockers to diagnosis, from our experience as a provider in the reproductive health space, are the lack of education amongst GPs,” she says. “Our recent report revealed that as a primary point of care, GPs need to be educated more on this disease and understand the referral process – which is why arming yourself with the NICE guidelines and Quality Statements is the best thing you can do when presenting for your first GP appointment.”
The fertility impact
Trying to conceive (TTC) is a main concern for many with endometriosis. While some are able to conceive naturally or with the help of fertility treatments, “it is estimated that 30-50 per cent of women with endometriosis experience fertility issues”, says Jenny. “Endometriosis can impact fertility, although the degree to which it presents varies from woman to woman. The condition causes inflammation, scarring, and the formation of adhesions within the pelvic cavity, which can impair the function of the ovaries, fallopian tubes, and uterus. In more severe cases, these physical changes can prevent egg release, block sperm from reaching the egg, or interfere with implantation.”
The report gathered vital information around the experience of trying to conceive from respondents. The key impacts highlighted by those surveyed include:
- Egg quality: can be significantly diminished by endometriosis, accelerating fertility decline beyond what is expected with age alone
- Implantation issues: the uterine environment can be compromised, making it harder for embryos to implant successfully
- Ovulatory dysfunction: endometriomas and scarring can inhibit ovulation or block fallopian tubes, preventing conception entirely
- Inflammation: even in the absence of pain, inflammation can be present and negatively affect fertility outcomes
- Increased miscarriage risk: poor egg quality and uterine complications associated with endometriosis can increase the likelihood of pregnancy loss.
“Many individuals only discover the full impact of endometriosis when struggling to conceive, highlighting the urgent need for earlier fertility education and proactive treatment,” says the report. A combination of medical, surgical and lifestyle interventions were often undertaken in the fertility journey.
However, Endometriosis UK wants to assure those with the disease that spontaneous pregnancy is still possible. “Endometriosis does not necessarily cause infertility, but there is an association with fertility problems, although the cause is not fully established,” says Faye. “Due to a lack of research, the links between fertility and endometriosis are not fully known.” The chances of conception will also vary depending on the severity of one’s endometriosis.
“If you are trying to conceive and you believe you have endometriosis, it is advised you see your GP sooner than the one year of recommended trying to conceive. This should advance your referral pathway for treatment,” says Jenny.
The psychological side
Considering the combination of chronic pain, frustration at not reaching a diagnosis, and worrying about the potential – or reality – of implications on fertility, it is no wonder that there is huge emotional strain that accompanies the condition. “The emotional toll of endometriosis can be profound and often underestimated. From our report, we know that chronic pain, fatigue, and the unpredictability of symptoms can severely affect daily functioning, relationships, and self-esteem,” says Jenny.
“Many sufferers experience anxiety, depression, and feelings of isolation, particularly if their symptoms are dismissed or misunderstood by others, including healthcare professionals.”
Of the respondents surveyed in the report, only five per cent felt like they’d received adequate medical support for fertility concerns, with 50 per cent feeling dismissed and unsupported.
There is also the reality that the severe pain and other symptoms cause sufferers to miss time at work or hours where they are able to be productive. “On average, they lose between 4.4 and 7.4 hours per week due to illness-related absences,” says the report. This can be a major – and frustrating – source of stress, with sufferers having to relinquish time unwillingly.
“The lengthy diagnostic journey and the potential impact on fertility further compound psychological distress. Managing a condition with no known cure can be overwhelming, especially when treatments provide only partial relief. Access to psychological support, peer networks, and empathetic care is crucial to improving the overall wellbeing of those living with endometriosis,” says Jenny.
The report showed that 29 per cent of respondents found their biggest solace in seeing a specialist, whilst 66 per cent of people found online communities and social media to be their most helpful support. While it is fantastic that these communities exist and sufferers have found them to be useful, the healthcare system should be providing them with the guidance, resources and support that they need.
“I have stage 4 endometriosis. When I was on the long journey to have that diagnosis, I was admitted to A&E due to the pain on four occasions. Since then, I have had two pregnancies. Whilst postpartum, after each pregnancy, I’ve experienced both a flare-up of symptoms and then a complete absence of them. The disease is so poorly understood, and here at OVUM, we strongly welcome more research and funding into this area of women’s health,” explains Jenny.
An investment and commitment to delivering endometriosis care at the highest level is imperative to improving the experiences of sufferers, as well as their futures. “Government must urgently commit to reducing non-cancer gynaecology wait times in line with the commitment made in the Autumn Budget to ensure patients wait no longer than 18 weeks from their referral to getting treatment – and to ensure that the estimated 1.5 million [people] in the UK with endometriosis are given due priority,” says Faye.
"Without access to diagnosis and treatment, not only can the disease progress, but it can have a negative impact on all aspects of someone’s life including their mental health, education and employment.”
Pharmacy’s role: how you can help
The 2025 Endometriosis Report by Ovum emphasises the importance of being familiar with the National Institute for Care Excellence’s (NICE) guidelines to improve endometriosis care, as well as Quality Standards for Endometriosis, which are issued where the NICE guidelines have not been implemented. As pharmacy team members help customers on their path to diagnosis, ensuring customers understand these guidelines is the first step.
“We have found there is a lot of variability in how much care providers know and understand [of] what they’re supposed to help you with,” says the report. “Although it is frustrating to have to advocate for yourself and do this homework, right now, it’s the best way to ensure you receive the care you need within the confines of the NHS.”
Pharmacy teams should also recommend, as the report does, keeping a pain and symptom diary – it may help you to be taken more seriously by a healthcare professional when you get to your appointment. Seeing the dates and patterns of symptoms may help accelerate the journey to diagnosis.
Advise customers not to “downplay [their] symptoms” suggests the report. “It’s essential to be transparent and honest about the level of pain you are experiencing, of the heaviness of your periods, for example. This is not the time to brush things off.”
Recently, the UK charity Wellbeing of Women launched their Period Symptom Checker to help women’s concerns be taken seriously when visiting the GP for period pain. It is a free, online survey. At the end of the survey, customers will be given recommendations on whether they should see a GP and if so, provide a printable copy of the symptom checker to substantiate the concern.
Follow this link to learn more about PCOS.